When it comes to anal fistulas, one of the most frequently asked questions is whether they are contagious. This condition, which affects the area around the anus, can be painful and distressing, leaving people to wonder if it can spread from person to person. In this blog, we will explore the truth behind anal fistulas, break down common myths, and provide you with essential information on the causes, symptoms, and treatment options.
Understanding anal fistulas and their contagiousness is crucial for those who are dealing with this condition or know someone who is. In the following sections, we will address some of the most common misconceptions and provide answers based on medical facts.
What Is an Anal Fistula?
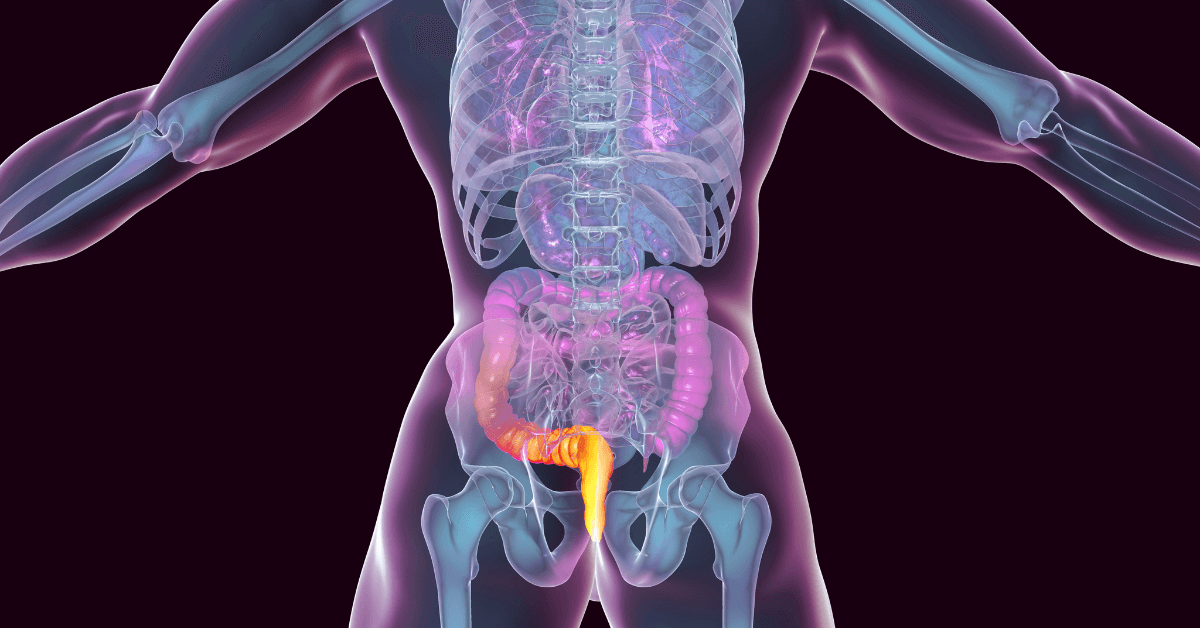
Before we dive into the question of whether anal fistulas are contagious, it’s essential to understand what an anal fistula is. An anal fistula is a small tunnel that forms between the skin near the anus and the inside of the anus or rectum. This condition typically develops as a result of an infection in the anal glands, which can lead to an abscess. When the abscess fails to heal properly, it can form a fistula.
An anal fistula can cause a variety of symptoms, including:
- Pain or discomfort around the anus
- Swelling and redness in the affected area
- Foul-smelling discharge
- Itching or irritation
- Fever in some cases (especially if the fistula becomes infected)
These symptoms can vary in severity depending on the size and location of the fistula. While an anal fistula can cause significant discomfort, it is not typically a life-threatening condition. However, it does require medical attention for proper diagnosis and treatment.
Are Anal Fistulas Contagious?
Now, let’s address the burning question: Are anal fistulas contagious? The simple answer is no—anal fistulas are not contagious. You cannot catch an anal fistula from someone else, nor can you spread it to others. This condition is not caused by a virus, bacteria, or any other infectious agent that can be transmitted from person to person.
The primary cause of an anal fistula is an infection in the anal glands, which leads to the formation of an abscess. If the abscess fails to heal on its own, it can develop into a fistula. This process is not contagious and occurs due to factors such as poor hygiene, chronic inflammation, or an underlying medical condition like Crohn’s disease.
Understanding the Causes of Anal Fistulas
Although anal fistulas themselves are not contagious, it is important to understand the underlying causes of this condition. By knowing what contributes to the development of anal fistulas, you can better prevent or manage the condition.
1. Infection and Abscess Formation
The most common cause of an anal fistula is an infection in the anal glands, which are responsible for secreting fluids that help lubricate the anus. When these glands become blocked or infected, an abscess can form. If the abscess does not drain or heal properly, it can create a tunnel or fistula between the anus and the skin.
2. Chronic Inflammatory Conditions
Conditions like Crohn’s disease or ulcerative colitis can lead to inflammation of the intestines and the anal area. Chronic inflammation in the anal region increases the likelihood of developing abscesses and fistulas. Individuals with these conditions are at a higher risk for recurrent anal fistulas.
3. Trauma or Injury
In some cases, an anal fistula may develop after an injury to the anal area, such as from surgery, childbirth, or an accident. Any damage to the skin around the anus can result in the formation of a fistula if it becomes infected.
4. Poor Hygiene
Poor hygiene practices can also contribute to the development of anal fistulas. Bacteria can accumulate around the anus, leading to infections in the anal glands. Regular cleaning of the area and proper hygiene can reduce the risk of infection.
Common Myths About Anal Fistulas
When it comes to anal fistulas, there are several myths and misconceptions that need to be addressed. Let’s debunk some of the most common myths:
Myth 1: Anal Fistulas Are Sexually Transmitted
One of the biggest misconceptions about anal fistulas is that they are sexually transmitted. This is false. Anal fistulas are not caused by any form of sexual contact, including anal sex. As mentioned earlier, they develop as a result of infection in the anal glands, not from an external pathogen or sexually transmitted infection (STI).
Myth 2: Anal Fistulas Are Caused by Poor Hygiene
While poor hygiene can increase the risk of developing an anal fistula, it is not the sole cause. Many people with good hygiene practices may still develop anal fistulas, particularly if they have underlying conditions like Crohn’s disease or have experienced trauma to the area. Maintaining proper hygiene is important, but it’s not a guarantee against developing anal fistulas.
Myth 3: Only Older Adults Get Anal Fistulas
Although anal fistulas are more common in adults, they can occur at any age, including in children and teens. Adolescents may develop anal fistulas due to infections, injury, or certain medical conditions. The idea that anal fistulas are a problem only for older adults is simply not true.
Myth 4: Fistulas Are Always Painful
Not all anal fistulas cause pain. Some people with anal fistulas may not experience any symptoms, especially if the fistula is small or not infected. However, when an infection is present, pain, swelling, and discharge are common symptoms. It’s important to remember that not every anal fistula results in pain or discomfort.
Symptoms of Anal Fistulas
Recognizing the symptoms of an anal fistula is important for early diagnosis and treatment. Some of the most common symptoms of anal fistulas include:
- Pain or discomfort around the anus: This is especially noticeable when sitting or moving.
- Redness or swelling: Infected fistulas may cause visible swelling or redness in the area.
- Foul-smelling discharge: If the fistula becomes infected or is draining, it can produce a foul-smelling pus or fluid.
- Itching or irritation: The skin around the anus may become irritated due to the drainage from the fistula.
- Fever: In cases of infection, a fever may develop as the body fights off the bacteria.
If you experience any of these symptoms, it is essential to consult with a healthcare provider for an accurate diagnosis and appropriate treatment.
Treatment Options for Anal Fistulas
While anal fistulas are not contagious, they can cause significant discomfort and may require treatment. There are several treatment options available, ranging from conservative methods to surgical intervention. The appropriate treatment depends on the severity of the fistula and the individual’s overall health.
1. Conservative Treatment
In some cases, conservative treatments such as warm sitz baths, antibiotics, and pain relievers can help manage the symptoms of an anal fistula. These treatments are typically used when the fistula is small, not infected, or causing minimal discomfort.
2. Surgical Treatment
For more severe or persistent cases, surgery is often required to remove the fistula. Surgical options include:
- Fistulotomy: The most common surgery for anal fistulas, in which the fistula tract is cut open to allow it to heal.
- Seton Placement: A seton is a piece of surgical thread placed through the fistula to help drain the infection and promote healing.
- Flap Surgery: In cases where the fistula is complex or near the sphincter muscles, flap surgery may be used to repair the area and close the fistula.
3. FiLaC®
FiLaC® (Fistula-tract Laser Closure) is a minimally invasive treatment for anal fistulas that uses a laser to close the fistula tract, promoting healing from the inside out. This procedure is performed under local anesthesia, offers a quicker recovery time, and is especially beneficial for complex or recurrent fistulas. It is less invasive than traditional surgery, reduces pain, and allows patients to return to normal activities sooner with a lower risk of complications.
Preventing Anal Fistulas
While not all anal fistulas can be prevented, there are steps you can take to reduce the risk of developing one. These include:
- Maintaining good hygiene: Clean the anal area gently but thoroughly to prevent infection.
- Managing underlying conditions: If you have conditions like Crohn’s disease or ulcerative colitis, work with your doctor to manage inflammation and prevent fistulas from forming.
- Avoiding injury: Protect the anal area from trauma, especially during activities like childbirth or surgery.
Conclusion
In conclusion, anal fistulas are not contagious, and the myth that they can be spread from person to person is simply false. They develop as a result of infections, chronic conditions, or trauma, not from an external infectious agent. While anal fistulas can cause significant discomfort, they can be treated effectively with medical care and proper hygiene practices.
If you suspect you have an anal fistula or experience any of the symptoms described, it’s important to seek medical advice to determine the best course of action. Schedule a consultation to speak with our providers to get personalized advice and treatment options. Understanding the facts about anal fistulas and their treatment options will help you manage the condition and improve your quality of life.